Translate this page into:
Ascher’s syndrome - A case report and review of literature
*Corresponding author: S. Akhilesh, Department of Emergency Medicine, Kauvery Hospital, Bengaluru, Karnataka, India. aakhilesh999@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Petkar K, Akhilesh S. Ascher’s syndrome - A case report and review of literature. Karnataka Med J. 2023;46:20-3. doi: 10.25259/KMJ_8_2023
Abstract
A condition characterised by double upper lip, blepharochalasis, and non-toxic thyroid swellings is called Ascher’s syndrome. Here, the author presents a case of Ascher’s syndrome with a relevant literature review.
Keywords
Ascher’s syndrome
Double lip
Blepharochalasis
INTRODUCTION
A congenital deformity characterised by loose mucosal folds in the upper lip studded with salivary glands present as a double upper lip. It is a major cosmetic embarrassment to the subject as also a functional nuisance while talking, eating, and performing oral hygiene. The condition is often associated with bilateral blepharochalasis with or without thyroid swellings when it is called Ascher’s syndrome. The condition is easily correctable surgically with satisfactory results. A patient with a double upper lip and bilateral blepharochalasis was managed by the author and is discussed here.
CASE REPORT
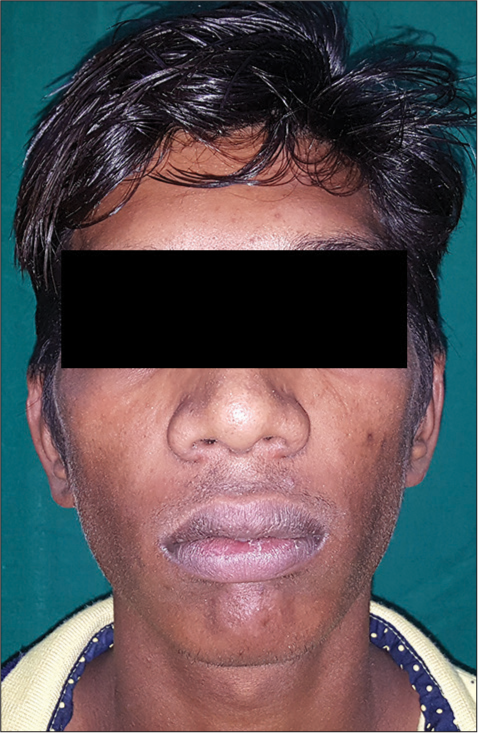
A 23-year-old male presented with cosmetic disfigurement of his face due mainly to a bulky upper lip that appeared to him and others as hiding a second lip. On repose, it looked like a bulky lip, while on splitting the lips or opening the mouth, a second upper lip would appear. There was no family history of similar deformities. On examination, he had a double upper lip due to loose and overhanging upper lip mucosa on either side of the frenulum with a normal, if not constricted, frenulum [Figures 1-3]. The patient also had drooping upper lids with excess skin folds [Figures 1-3]. The patient was unhappy about the upper lids, too, as they gave him a tired and aged look. A thorough clinical examination revealed no thyroid swellings. His other general and systemic examinations were unremarkable. All his routine investigations and thyroid function tests were normal.

- Drooping upper eyelid with excess skin folds and Bulky double lip appearance.

- Loose overhanging upper lip on splitting the lips.

- Double upper lip on either side of frenulum.
The patient underwent upper lip reduction and bilateral blepharoplasty in one sitting under local anaesthesia.
Upper blepharoplasty markings were made with an extension over the lateral orbital margin to address severe lateral hooding. The lower marking was made 10 mm from the lid margin. The excess lid skin was caught with plain forceps without causing stretching or ectropion while gently closing the eyes, and an upper marking was made. For the upper lip reduction, separate elliptical excision markings were made on either side of the frenulum. The anterior border of the marking was about as far from the white roll medially as the thickness of the lip at the frenulum, tapering towards the commissure. The extra mucosa that could be grasped with fingers was assessed, and the posterior border was marked. The medial end of excision was about 2 mm from the frenulum, without cutting the frenulum, and laterally, the markings extended approximately 2 mm beyond the commissure onto the upper buccal mucosa [Figures 4 and 5]. The markings were made in sitting posture.

- Upper blepharoplasty markings.

- Elliptical excision markings on either side of frenulum.
Xylocaine with adrenaline infiltration was made into both upper lids using a 26-G needle. Blepharoplasty was performed by first excising skin and a strip of preseptal orbicularis oculi up to the septum [Figure 6]. The septum on either side was breached, and herniating fat was clamped, trimmed by scissor excision and cauterised. Closure was done by a single layer of non-absorbable suture – continuous medially and interrupted laterally. Steri-strips were placed over the sutures.

- Blepharoplasty - Excision of skin and pre-septal or orbicularis oculi.
Bilateral infra-orbital nerve blocks were given. About 5 min later, submucosal infiltration was made under the marked area of the upper lip with Xylocaine containing adrenaline using a 26-G needle. Excision was started about 10 min later. The deeper (posterior) border was first incised. The mucosa, along with salivary glands was dissected off the orbicularis oris muscle to elevate a mucosal ‘flap’ base on the anterior border of the marking [Figure 7]. The reach of the mucosa for closure was ascertained, and the anterior border was redrawn as necessary and was cut with scissors. The mucosal cut ends were sutured with absorbable interrupted sutures. The procedure was completed on the one side before proceeding to the other side to note and record the difference [Figure 8].

- Excision of excess posterior mucosal flap.

- Post-posterior mucosal excision.
Post-operatively, the patient received antibiotics and analgesics, along with cold compresses. The upper lid sutures were removed on 4th postoperative day.
Post-operative results, as assessed at 2 weeks from surgery, were satisfactory for the patient and his family [Figures 9 and 10]. The upper lid crease gave him a youthful look. The bulk and the curvature of lip borders were satisfactory. Although there was a mild asymmetry of the lips, the patient’s mother was happy as it looked more natural than having a symmetrical lip.
- Post-operative assessment after 2 weeks.

- Satisfactory upper lip curvature.
DISCUSSION
A condition involving double upper lip, blepharochalasis and non-toxic thyroid swellings was described by Ascher, an ophthalmologist in 1920.[1] The thyroid swellings are rare and are not required to make a diagnosis of theAscher’s syndrome. Other related conditions described include iris coloboma, heterochromia iridum narrowing of the horizontal palpebral fissure, and decreased outer intercanthal distance secondary to the lengthening of lateral canthal ligament.[2] Parmar and Muranjan have described another syndrome with double upper and lower lips, hypertelorism, ptosis, blepharophimosis, and clinodactyly.[3]
The double upper lip is so rare an entity that there are only reports of a few cases in literature with hardly any larger series. Its prevalence is difficult to note, but it seems to have a male predilection. A double lower lip is also described and can co-exist with a double upper lip, too. TheAlthough it is a hitherto harmless clinical condition, one should rule out a troublesome vascular lesion as the same can present as a double lip.[4] It is important to suspect ascher’s syndrome in people with double upper lip as patient may present mainly with other complaints like dysphagia, dysarthria etc rather than complaining of double lip. Treatment of this condition is surgical. As with blepharoplasty, lip reduction is also done mainly for cosmetic reasons. The techniques often used are elliptical excisions on either side of the frenulum, single ellipse excisions across the width of the upper lip, and W-excisions. A tight frenulum, when there is one, needs to be elongated by a manoeuvre like a Z-plasty.
Because of the rarity in the presentation and reporting of this condition, awareness of this entity and its management options seems to be less among the medical fraternity. A compilation of all the literature available on double lips and Ascher’s syndrome is needed to draw management protocols.
CONCLUSION
Ascher’s syndrome is a rare condition seen in everyday medical practice. Because of this rare presentation and reporting, it is essential to the medical team to be made more aware of this condition of better diagnosis and management.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial Intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Double lip surgical correction in Ascher's syndrome: Diagnosis and treatment of a rare condition. Clinics (Sao Paulo). 2008;63:709-12.
- [CrossRef] [PubMed] [Google Scholar]
- Ascher's syndrome: A rare case report. Indian J Ophthalmol. 2015;63:264-7.
- [CrossRef] [PubMed] [Google Scholar]
- A newly recognized syndrome with double upper and lower lip, hypertelorism, eyelid ptosis, blepharophimosis, and third finger clinodactyly. Am J Med Genet. 2004;124A:200-1.
- [CrossRef] [PubMed] [Google Scholar]
- Double lip deformity secondary to the hemangioma. Anatol J Clin Investig. 2013;7:222-4.
- [Google Scholar]






